Antimycobacterial Agents
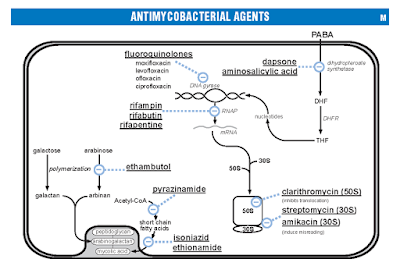
Historically, mycobacterial infections have been associated with signifi cant morbidity and mortality worldwide. In particular, Mycobacterium tuberculosis is a highly successful human pathogen, infecting one-third of the world’s population and leading to approximately 3 million deaths worldwide annually (1). The organism is unique in its ability to establish persistent infection, requiring prolonged treatment with antimicrobials in order to achieve clinical cure. In general, the goals of antituberculosis therapy include rapid reduction of the massive numbers of actively multiplying bacilli in the diseased host, prevention of acquired drug resistance, and sterilization of infected host tissues to prevent clinical relapse. In order to achieve these goals, currently accepted guidelines recommend administration of multiple active drugs for a minimum duration of 6 months (2). In areas where drug resistance is prevalent and resources permit, M. tuberculosis clinical isolates should be...